1234567890
prn8099 - Number 10, October 1996
POISON PREVENTION THROUGH QUALITY INFORMATION
Dzulkifli Abdul Razak
As the saying goes: Prevention is better than cure. This adage has withstood the test of time and according to some it has been around even before the time of Socrates. Especially for those who are involved in the promotion of health, it is perhaps a cornerstone in much of their effort to deliver health care to the people. Simple as it is, the saying makes good sense in our attempt to remain healthy for the good part of our lives. This is more so today when the social and economic structures of the country are rapidly changing to suit the pace of industrialisation. In the process, at times, the toll on health is indeed very high. And without the proper preventive action it can only get worse. For example, it was revealed lately that the number of industrial mishaps, especially death at the workplace has been increasing since 1990. And in majority of these cases, it can almost be assumed that the proper preventive action is either not fully understood or having totally neglected.
| Year | Accidents | Deaths |
|---|---|---|
| 1990 | 121,104 | n.a |
| 1991 | 124,898 | n.a |
| 1992 | 130,019 | 541 |
| 1993 | 133,293 | 653 |
| 1994 | 122,688 | 644 |
| 1995 | 114,134 | 925 |
With rapid industrialisation and urbanisation currently taking place in the country, occupational diseases as well as those related to environmental pollution are also becoming more common. There is already a raising concern over the quality of workplace that one regularly comes in contact with. Given the fact that the workers today are more exposed to an even larger assortment of industrial chemicals and wastes, this report the number of work-related diseases is also alarming.
| Year | Incidences |
|---|---|
| 1990 | 77 |
| 1991 | 502 |
| 1992 | 2,942 |
| 1993 | 1,026 |
| 1994 | 1,045 |
On a broader scope of course, the same axiom applies equally well to the aspects of environmental health, which is becoming more important today. Noxious fumes, gases and other pollutants spewed into the air are known to affect health in a multitude of ways especially for those suffering from asthma and other respiratory illnesses, as well as causing undue irritations to the skin and eyes. This time, unfortunately, the damage could extend beyond the workplace, affecting the population at large. Water and land pollution further add to the already deteriorating situations notwithstanding the efforts and measures put in place by the various government agencies. We only need to keep reminding ourselves of the various tragedies that occur in recent years in Malaysia to have a fair idea of the dimension that would continue to confront us in the near future if we are not caring enough.
What is apparent in all these situations, however is the fact that they are all preventable. Another equally important point to note perhaps is that information is pivotal in preventing every one of them. As much as the need for information is as crucial as in wanting to accurately diagnose and treat each of these cases; its usefulness too cannot be overemphasised if preventive actions are to have any meaningful impact. For example, information is important in any programme of preventive education be it for the workers, employers, professionals or the lay public; similarly information is also essential if we want to create a level of awareness for more effective follow-up preventive activities. Information too is necessary in the drafting up of long-term plans and strategies, including monitoring and interventions. However, it is not just the issue of information per se, but more importantly the question of accuracy, reliability and expediency of data, as well as their accessibility and availability to all those who require them. It is invariably related to the issue of the quality of information exchanged and utilised in the attempt to improve the overall health care status given today's pace of development. This is imperative if viewed within the context of the challenges of Vision 2020, whereby Malaysia is to be not only a nation that is information-rich, but at the same time, stands proud of its health and health care status. After all, "good data" and information is very much a prerequisite to "good" health.
The emerging challenges therefore are directed at building a comprehensive data set and information pool especially in situations where there has been very little data collected or the total lack of it. Where there is already substantial information being kept there may need to be a mechanism of how it can be shared especially where more than one agencies are involved. More importantly, in so doing there will be no need to jeopardise the question of confidentiality and privacy in the process. While 'secrecy' has its place in protecting the rights of the individuals, it must not be allowed to overshadow the common good that could be derived in making such data or information available.
In the context of poisoning, commonly the outcome of occupational and enviromental hazards, the relaying and sharing of quality information are indeed crucial. Pusat Racun Negara, in cognisant of this fact has, since its inception paid particular attention to the need of creating an openness towards information-sharing and exchange. By setting up two specific components namely Drug and Poison Information Services, and Research and Documention Services, PRN sets out to promote just that.
Under the Drug and Poison Information Services, the objectives are:
- to function as the main resource centre in providing information on toxicity and risk of poisons.
- to assist in the mangement of poisoning cases
- to systematically disseminate drug and poison information, and advise through the use of efficient, reliable and cost-effective methods; whereas for the Research and Documentation Services, they are:
- to compile information on poisonous substances on a continuous basis.
- to develop computer applications in order to facilitate information transfer and use by the Drug and Poison Information Services.
- to research into systematic collection of poisoning data and information through toxicovigilance and toxicokinetic studies.
To further optimise the utilisation and documentation of information, the two services are further integrated with the other components of PRN, namely, the Poison Education and Prevention Services, and of late Toxicology Laboratory Services. Each of the other services also assist in information-sharing and exchange activities via various activities like publications of its own bimonthly bulletins (PenawaRacun & PRN8099), publishing series of articles/questions and answers in three major dailies, organising a biweekly radio talkshow (courtesy of RTM Penang) and also participating in exhibitions and seminars for professionals as well as the public. On top of these, PRN devoted a special toll-free line (800-8099) for use of everyone who is in need of assistance from the Centre, especially during emergencies. In fact currently this has been the main mode of communication for the request of poisoning information from PRN. To facilitate meaningful data capture for documentation, PRN devised a special format to be used when referring poisoning cases to PRN. This format is being widely circulated to all practising professional through the quarterly issue of DIMS since 1995.
In the attempt to make information more readily available and create a high level of health awareness among Malaysians, PRN launches its own homepage - Malaysian Drug & Poison Net, (PRN-Net for short) in April 1996. With the rapidly developing information highways like the Internet, PRN believes that there is a real need for information to be shared with people of all walks of life, regardless of their educational and professionals levels. In this way, the homepage also addresses, at least in part, the concern for information equity by serving as a gateway for all those interested to gain quick access into information on poisoning and health placed therein. In the same breath it acts as an interface to many of the information sources available on the Internet so that the dissemination of relevant information be widely spread among Malaysians. In this sense PRN acts as a global link for easy retrieval of good information, while helping to keep the cost of access affordable. On certain occassions, the Internet too has proved invaluable as an information-sharing tool in solving some of the more complex cases. Further computerised projects, including the use of artificial intelligence (AI) are now under way to reinforce this effort.
The emerging role of the Internet in this regard has been an eye-opener, increasingly recognised even at international level. As late as April 1995, Internet has been called upon to rescue to an unsuspected poisoning case in Beijing in what is now homepaged as "The First International Telemedicine Trial to China: Zhu Ling's Case"
The Case Summary: The patient is a 21-year old female student studying at Peking [sic] University. She became sick in the later part of 1994 and then hospitalised. After being somewhat treated, she again became very sick and was re-admitted. Her case was not completely diagnosed by the local doctors despite a number of tests being carried out. She went into coma in March 1995. It was not until April 10, 1995 that an SOS message appeared on the Internet requesting for help sent by her colleague at the University. Barely a few days later, professionals and experts the world over came to the rescue giving medical opinions and suggestions as to the case via the Internet. Based on the feedback, in less than three weeks later, the patient was confirmed to suffer from thallium poisoning - some 50 times more than the normal level in the body. Following further communications between experts and the Chinese counterparts the appropriate treatments were insituted about a week later. The patient came out of coma at the end of August 1995, after almost a six-month period. She is now reported on the way to recovery thanks to the Internet. The full documentation of the case can be retrieved from the Internet including visuals of the patient (before and after), her CT and MRI scans as well as the chronology of events.
Source: Internet, http://www.radsci.ucla.edu/telemed/zhuling
The above documentation is not only an interesting medical case in itself but also provides important lessons about information-sharing and exchange more specifically about poisonings. Firstly, it involves not just the professionals but also the lay public as they are now more aware and knowledgeable. In this case it is the student who initiated the SOS message (apparently much to the chagrin of the professionals concern) and sparked off the life-saving episode. The rest is now history. Secondly, it is also clear from this unique experience that electronic information-sharing (read "rapid and accurate") can save lives and is surely the way forward if properly conceptualised. Thirdly of course is that there are information that could be shared by all parties - patients and professionals - and that there is a willingness to do so. The out-moded attitude that "information is power" can only serve as a stumbling block and must be dispensed away in the interest of health. It important to reiterate that in matters of health care to derive "power" by wholesale embargo (read "sulit"), or hoarding pertinent bits and pieces of information that could in essence improve and better health outcomes is at least unprofessional if not outright unethical. Similarly the prevailing apathy in reporting such cases on part of those involved can no longer be tolerated because it is equally irresponsible, more so when lives are at stake.
Such lessons are even more pressing in cases of poisonings because we still lack a reliable baseline data for the entire country. Pusat Racun Negara believes that even when all the statistical data for poisoning nationwide are combined together, it is still far from giving the true picture. We have yet to have a representative data set that could be used with confidence fairly reflective of the situation in the country. Going by the experience of the industrialized countries, the estimated annual penetrance rate of poisoning is about 6 to 7 per 1,000 population. Using a conservative estimate of about 1 per 1,000 population for countries like Malaysia, there are at least about 20,000 poisoning cases nationwide and the number is bound to increase with time. Needless to say we have still a long way to go in reaching the majority of the population in effectively tackling the problem at hand. However, the experiences of PRN in the last two years indicated that there is still a lot of room for improving the situation.
In this respect there should be a comprehensive nationwide information network for poisoning. The poison network could serve as an excellent mechanism for information-sharing and exchange. With the advent of a variety of infocommunication tools now taking place and some fast becoming common features in many health institutions and organisations, information-sharing and exchange ought to be adopted as yet another positive approach to increase the health standards across the board. In this way a more systematic and coordinated effort could be undertaken, where the notifications of poisonings or other massive chemical accidents can be notified and speedily dealt with in collaboration with the appropriate agencies to prevent and control the incidents from escalating. Efficient infocommunication systems can create not only reliable early warning systems but also allow the appropriate responses to be devised to prevent an incident from getting out of hand. In short it can also function as a focal point on any matters relating to poisoning information, ranging from the collection, collation, compilation, documentation and dissemination of poisoning information. By and large the network will a basis for creating a sufficiently strong large databases that could eventually help in determining patterns, trends and relationships between the various possible indicators in order that the prevailing situations be better understood. This in turn is an invaluable contribution towards planning and deciding the course of future preventive actions.
Pusat Racun Negara looks forward to such an efforts as complementary to its mission, namely "to reduce the mortality, morbidity, occurrence and cost of poisoning in a manner that strives for excellence, compassion and innovation." Thus, PRN remains committed to collaborate with any partner that shares similar aspirations. Unless and until some collective effort is taken in a concerted way, it can only mean that we are prepare to waste much more of our precious resources, including that of human lives, as the country advances into greater heights. On the contrary by being proactive today, much of the impending tragedies could be spared and the resources be put to better use in proctecting ourselves and our environment. Only then can we say that we lived up to the age-old saying, prevention is indeed better than cure.
PRN CONSULT 
Review on ORGANOCHLORINE INSECTICIDES
Mohd Isa Abd. Majid, PhD
Introduction
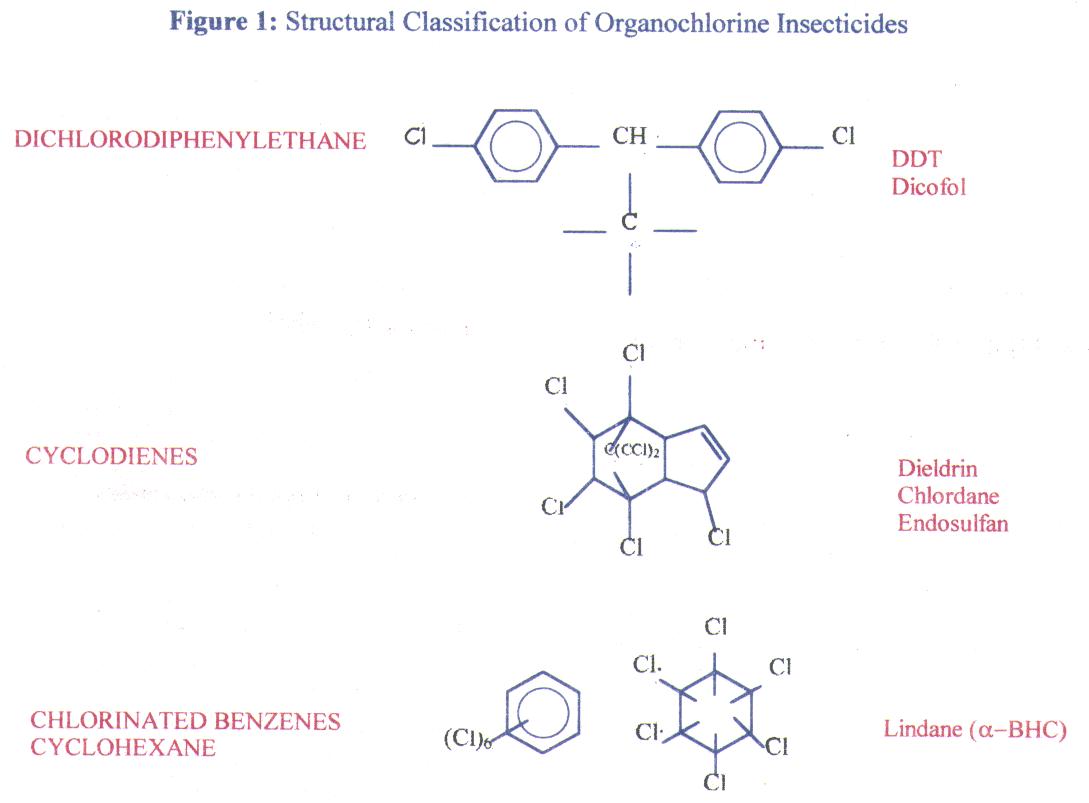
The organochlorine (chlorinated hydrocarbon) insecticides are a diverse group of agents belonging to three distinct chemical classes including the dichlorodiphenylethane-, the chlorinated cyclodiene- and the chlorinated benzene and cyclohexane-related structures as shown in Figure 1. These compounds have been used extensively from mid-1940s to the mid-1960s in all aspects of agriculture and forestry, in building and structural protection and in human situations to control a wide variety of insect pests. Their well known properties (low volatility, chemical stability, lipid solubility, slow rate of biotransformation and degradation) that made these compounds such effective insecticides also brought about their restricted uses nowadays because of its persistence in the environment, accumulated concentrations within various food chains and the magnification of biological active body bioburdens in many wildlife species that interfered with the reproductive success of the species.
What are the available organochlorine insecticides in Malaysia?
The various approved pesticide products that contain organochlorine insecticides are listed in Table 1.
Table 1: Registered products containing organochlorine insecticides
(Source:Pesticide Board of Malaysia - List of Registered Pesticides 1992-1994)
| Dichlorodiphenylethanes | ||
| Product | Active Ingredient | Concentration (%w/w) |
|---|---|---|
| Acathane | Dicofol | 18.7 |
| DDT Teknikal | DDT | 70.0 |
| Didity | DDT | 70.0 |
| Didity 25EC | DDT | 17.5 |
| Gold Coin DDT EC | DDT | 17.5 |
| Gold Coin DDT WP | DDT | 55.5 |
| Kelthane EC | Dicofol | 18.5 |
| Meto | Dicofol | 18.7 |
| Trithane | Dicofol | 18.7 |
| Cyclodienes | ||
| Acmaron 35EC | Endosulfan | 35 |
| Acmaron 3G | Endosulfan | 3 |
| Acmaron Technical | Endosulfan | 94 |
| Ancom Endosulfan 33 | Endosulfan | 32.9 |
| CH Endosulfan | Endosulfan | 32.9 |
| CH Endosulfan 3G | Endosulfan | 3 |
| Chlordane Teknikal | Chlordane | 100.0 |
| CSH-Endosulfan 35 | Endosulfan | 35 |
| CSH-Endosulfan Technical | Endosulfan | 94.0 |
| D15 | Dieldrin | 15.9 |
| Dosul 35% | Endosulfan | 35 |
| Endocel Technical | Endosulfan | 94 |
| Endofan 350 | Endosulfan | 32.9 |
| Endol 35EC | Endosulfan | 32.5 |
| Endosulfan Technical | Endosulfan | 94 |
| Endosulfan Technical | Endosulfan | 94 |
| Endosulfan Technical | Endosulfan | 93 |
| Endosulfan Technical | Endosulfan | 95 |
| Endotox 555 | Endosulfan | 32.9 |
| Fezdion 35EC | Endosulfan | 32.9 |
| Gold Coin Fezdion 35EC | Endosulfan | 35 |
| Halex Endosulfan | Endosulfan | 35 |
| Harvest | Endosulfan | 32.9 |
| Kendan | Endosulfan | 32.9 |
| MAPA Endosulfan Tech | Endosulfan | 95 |
| Polydan | Endosulfan | 33.5 |
| Premofan 35EC | Endosulfan | 35 |
| Supersulfan | Endosulfan | 32.9 |
| Tengkorak 3500 | Endosulfan | 32.9 |
| Thiodan 3% Granular | Endosulfan | 3 |
| Thiodan 35EC | Endosulfan | 32.9 |
| Thiodan Technical | Endosulfan | 94 |
| WA Chlordane | Chlordane | 63.8 |
| WA Chlordane 30 | Chlordane | 30 |
| WA Chlordane SP | Chlordane | 74.2 |
| Zesdane | Chlordane | 30 |
| Chlorinated benzenes or cyclohexanes | ||
| ACM Lindane | Gamma BHC | 20 |
| ACM Lindane 4 WP | Gamma BHC | 4 |
| ACM Lindane 5% WP | Gamma BHC | 5 |
| ACM Lindane 6.5% WP | Gamma BHC | 6.5 |
| Ancom Lindane Flowable | Gamma BHC | 20.5 |
| Celcide 20 EC | Gamma BHC | 20 |
| Celcide Technical | Gamma BHC | 99.0 |
| CH Lindane 20 EC | Gamma BHC | 20 |
| Dol-G | Gamma BHC | 5 |
| Dolacide 6.5% WP | Gamma BHC | 6.5 |
| Gamma BHC 9.9 WP Chap Singa | Gamma BHC | 9.9 |
| Gammacide 400 | Gamma BHC | 4 |
| Gammexane 20 | Gamma BHC | 20 |
| Gold Coin Lindane 20 EC | Gamma BHC | 20 |
| Halex Lindane 20 EC | Gamma BHC | 20 |
| Hammer 20 EC | Gamma BHC | 20 |
| Lindacide | Gamma BHC | 6.5 |
| Lindacol | Gamma BHC | 50 |
| Lindan Technical | Gamma BHC | 99.4 |
| Lindane Technical | Gamma BHC | 99 |
| Lindane Technical | Gamma BHC | 99 |
| Lindane Technical | Gamma BHC | 99.5 |
| Lindicide | Gamma BHC | 6.5 |
| Lindox 20 EC | Gamma BHC | 20 |
| Lithane | Gamma BHC | 20 |
| MAPA Lindane 20 EC | Gamma BHC | 20 |
| MAPA Lindane Technical | Gamma BHC | 99.5 |
| WA Lindane 200 | Gamma BHC | 20.3 |
| ZM Lindane 20 EC | Gamma BHC | 20 |
They can all be absorbed by either inhalation or ingestion and in some situations by dermal absorption. The clinical effects following acute exposure to high concentrations are principally on the nervous system, although clinical findings may include headache, nausea, dizziness and irritability. In severe cases there may be weakness, ataxia, tremor, confusion, muscle fasciculation and peripheral parathesiae. Seizure and coma may follow severe poisoning with the cyclodiene compounds. The consumption of foodstuffs contaminated with organochlorines has been associated with a complex of signs and symptoms including headache, nausea, irritability, vertigo, muscle twitching, confusion, convulsions and coma.
There are no biological markers for poisoning by any of these compounds so that poisoning can only be confirmed by specific laboratory detection of the pesticide by analysis of biological specimens. Treatment is essentially symptomatic but may include decontamination. There are no specific antidotes and the serious toxic effects, such as seizures, should be treated appropriately. Some of these compounds are hepatotoxic and close monitoring of liver function should be maintained even after other biochemical changes have recovered.
What are the characteristics of each class of organochlorine insecticides?
A. Dichlorodiphenylethanes
- Dichlorodiphenyltrichloroethane (DDT)
DDT was first synthesized in the 19th century but was not used as an insecticide until the 1930s. As well as being one of the oldest synthetic pesticide it is probably also one of the most effective. Its use had a significant impact on the control of insect vectors of disease during World War II and use increase significantly until the early 1960s. At that time evidence suggested that many insect species were developing resistance to DDT and there was increasing concern that the pesticide was accumulating in the general environment and entering the food chain.
The main site of toxic action of DDT is on the nervous system. Acute exposure produces repetitive discharges of neurones which in acute poisoning may result in tremors, fits and ultimately paralysis and death. DDT affects the polarisation of excitable membranes and lowers the threshold for excitation. This effect is principally a result of interference with sodium and potassium conductance across the membrane and a failure to inactivate the influx of sodium ions at the end of a generated action potential and the efflux of potassium ions that is involved the depolarisation of the membrane. The continuing inflow of sodium ions further depolarises the cell membrane and may trigger another action potential. This cycle results in the repetitive neuronal discharges. Although DDT may be stored in all body tissues, the highest concentrations occur in adipose tissue. In man exposure to a dose of 10 mg per kg body-weight or above would be expected to produce acute toxic effects. These would include muscle weakness, tingling and numbness, and possibly convulsions. Dermal absorption of DDT is poor and the principal route of exposure is by oral ingestion.
B. Hexachlorocyclohexanes
- Gamma-benzene hexachloride (-BHC, lindane)
Another specific group of chlorinated hydrocarbon insecticides are the isomers of benzene hexachloride, (e.g. -hexachlorocyclohexane, lindane). The principal use of lindane is as a general insecticide. In man the main route of exposure are either by inhalation, skin absorption, or ingestion. The results of some animal toxicity tests have suggested that lindane may be carcinogenic, but case reports in man have suggested only a possible association in children of exposure to lindane and the development of a neuroblastoma. Chronic feeding of 800 ppm lindane to rats in their diet resulted in mild hepatic damage and some effects on renal function occurred at higher doses. Mice fed 400 ppm lindane in their diet developed liver tumours with, in a few cases, lung metastases. The powder form applied to the skin of rabbits caused only a moderate skin irritation.
Lindane is used for the treatment of scabies and head and body lice. It is usually available as a shampoo, lotion and cream. The shampoo which should be used for lice is to be applied as a 15-30ml dose in children or up to 60 ml in adults and left on for about 4 minutes. The cream and lotion which are used to treat scabies should be left on the body for eight to 12 hours. It should be applied in a thin layer and gently massaged into all skin areas except the face, eyes, mucous membranes and urethral meatus.
The clinical signs associated with acute lindane poisoning are similar to those of DDT, although the neuronal excitation may be more severe. The different steric isomers of hexachlorocyclohexane display differing degree of toxicity, the isomer is a nervous system excitant while the and isomers, produce nervous system inhibition. The neuroexcitatory action of the isomer may be due to inhibition of the pharmacological action of the neurotransmitter gamma-aminobutyric acid (GABA) by a mechanism similar to that of picrotoxin. The clinical findings include neurological effects such as repetitive clonic convulsions sometimes superimposed on continuous tonic spasms. A severe exposure can result in clonic convulsions with respiratory difficulties and cyanosis. Accidental ingestion of a large dose of lindane has caused death.
The signs and symptoms of acute exposure to lindane vapour in man include irritation of the eyes, nose and throat; severe headache; and often nausea. The results of chronic toxicity tests in animals have suggested that lindane may cause liver and kidney damage and skin irritation and that a long-term effect may be the development of aplastic anaemia. Lindane exposure has been suggested as a possible environmental cause of aplastic anaemia in man.
This association may, however, have been due to contaminants or thermal breakdown products, since in many of the case reports the source of exposure was a space vaporiser.
Plasma lindane concentrations do not appear to increase directly with the duration of exposure but to reflect recent lindane absorption. Workers exposed to air lindane concentrations of 31-1800 g per m3 were found to have blood lindane concentrations ranging from 1.9 - 8.3 ppb. The relative blood concentrations of the steric isomers of lindane of lindane (, , ,) have been suggested to be an indication of the history and extent of lindane absorption.
C. Cyclodienes
- Dieldrin
Aldrin and dieldrin are chlorinated cyclodiene insecticides that are considered to be amongst the most toxic and environmentally persistent pesticides. Following absorption, aldrin is rapidly metabolized to dieldrin, although both are capable of producing neurotoxicity. Their mechanism of toxicity is similar to that of DDT and involves interference with the movement of ions across excitable membranes. The cyclodienes are so well absorbed through the skin that their oral, inhalation and dermal LD50 values are very similar.
In man, dieldrin has an estimated blood elimination half-life of 8.5 months and, therefore, it would take more than 5 x 8.5 months, (i.e. over 3.5 years) for 95 per cent of any absorbed dieldrin to be eliminated from the blood.
Dieldrin is a volatile compound, and acute absorption by inhalation is associated with headaches, dizziness, nausea and vomiting, sweating, malaise, and lethargy. Severe poisoning can result in neurological signs such as myoclonic jerks or convulsions and ultimately coma and even death. In 5 reported cases of serious occupational poisoning, blood dieldrin concentrations were around 620ppb (in a healthy group of workers the maximum blood concentration measured was 220 ppb).
In man it has been demonstrated that the fat: plasma dieldrin concentration ratios are 174:1 at 3 days and 2200:1 at 179 days after exposure, confirming the retention of the compound in body fat and suggesting that, with time, the plasma dieldrin concentration represents a diminishing fraction of the total body dieldrin burden. Dieldrin appears to be stored in body fat as the epoxide and is principally excreted by the kidney in urine.
- Chlordane
The use of chlordane in some countries is now severely restricted. Several reports have suggested that extensive exposure to chlordane over several weeks can be associated with the development of symptoms of anorexia, nausea, fatigue, malaise, and paraesthesiae. Heavy exposure during household use may have been linked to the temporary development of a megaloblastic anaemia, but it may be that there is a polymorphism for susceptibility to blood dyscrasias with organochlorine pesticides. The ingestion of 6g chlordane by an adult resulted in death and lower doses have caused seizures and stupor. Chlordane is excreted from the body in a few days and is secreted in breast milk. It is a potent inducer of hepatic enzymes and is stored in body fat. The fat: serum partition ratio in exposed workers was found to be 660:1.
What are the signs and symptoms of organochlorine poisoning?
Symptoms begin within 30 minutes to 6 hours after ingestion. Given the diversity of chemical structure for organochlorine, the sign and symptoms of toxicity and mechanism(s) of action are somewhat different. Table 2 summarises the signs and symptoms of acute and chronic toxicity following exposure to these chemicals. In general, nausea, vomiting and diarrhoea may precede CNS irritability or the latter may occur first. It has been reported that seizures can occur without the initial signs of CNS hyperexcitability.
Table 2: Signs and symptoms of acute and chronic toxicity following exposure to organochlorine insecticides
| Insecticides class | Acute signs | Chronic signs |
|---|---|---|
| Dichlorodiphenylethanes | Parathesia Ataxia, abnormal stepping Dizziness, confusion, headache |
Loss of weight Mild anaemia Tremors |
| Hexachlorocyclohexanes | Nausea, vomiting Fatigue, lethargy Tremor Nervous tension |
Muscular weakness EEG pattern changes Hyperexcitability, anxiety |
| Cyclodienes | Dizziness, headache Nausea, vomiting Motor hyperexcitability Hyperreflexia Myoclonic jerking General malaise Convulsive seizures Generalised convulsions |
Headache, dizziness, hyperexcitability myoclonic jerking Psychological disorders including insomnia, anxiety, irritability EEG pattern changes Loss of consciousness Epileptiform convulsions |
How is treatment being done in organochlorine poisoning?
There is no antidote for organochlorine poisoning and treatment is largely symptomatic in nature.
In confirmed organochlorine poisoning, cardiovascular and respiratory functions need to be supported. Following acute exposure, blood chlorinated hydrocarbons levels are not clinically useful as most compounds will show cumulative exposure over a period of months or years rather than recent exposure.
In cases of oral exposure, the management of organochlorine poisoning involves:
Respiratory support
Airway management is the first priority. Endotracheal intubation should be performed for respiratory failure and to protect against pulmonary aspiration.
Prevention of further absorption
Emesis is not recommended due to the potential CNS depression or seizures which may arise. As an alternative, gastric lavage using a large bore orogastric tube may be indicated if performed soon after ingestion or in patients who are comatose. Adequate seizure control is mandatory prior to gastric lavage. The gastric lavage is performed with 150 to 200 ml lukewarm tap water or saline per wash for adult and children above 5 years old and 50 to 100 ml of normal saline per wash in young children. The lavage is continued until the lavage return is clear. The volume of lavage return should approximate the amount of fluid given to avoid fluid and electrolyte imbalance.
Activated charcoal is also given to absorb the remaining organochlorine. Normally, this is administered in the form of aqueous slurry or mixture of charcoal with saline cathartic or sorbitol. The dose for activated charcoal is 15-30 gm for children while for adult 50-100 gm orally or by tube if the patient is awake and the airway is protected. The saline cathartic dose for adult is 20-30 gm per dose of magnesium or sodium sulphate or magnesium citrate 4 ml/kg per dose up to 300 ml per dose administered orally. For paediatric dose, 250 mg/kg per dose of magnesium or sodium or magnesium sulphate or magnesium citrate 4 ml/kg per dose up to 300 ml per dose is administered orally. In the case of sorbitol, the adult is 1-2 gm per kg per dose to a maximum of 150 gm per dose administered orally while for children over 1 year of age, a dose of 1 to 1.5 gm/kg/dose as a 35% solution to a maximum of 50 gm/dose is usually given.
To prevent further absorption from spillage onto the cloth, the decontamination process involves removing the contaminated clothing, washing the skin including the hair and nails vigorously and doing repeated soap washings. In addition, leather absorbs pesticides and hence leather should not be worn in the presence of pesticides and all contaminated leather should be discarded.
Providing treatment of arising problems
The life threatening situation in organochlorine insecticide poisoning is associated with tremors, motor seizures, and the interference with respiratory function (hypoxemia and resulting acidosis) arising from repetitive stimulation of the CNS. In cases of seizures occurring, administer diazepam intravenously over a period of 2 to 3 minutes. The adult diazepam dose is 5 to 10 mg initially which may be repeated every 10 to 15 minutes as needed to a maximum of 30 mg. For children, the normal recommended dose is 0.25 to 0.4 mg per kg up to a maximum of 5 mg in children 30 days to 5 years and a maximum of 10 mg in children over 5 years. If seizures cannot be controlled with diazepam or recurring, administer phenytoin according to the usual dose.
In certain organochlorines especially the slowly excreted organochlorines such as chlordane, the oral administration of anion- exchange resin, cholestyramine, to intoxicated patients resulted in 3 to 18 fold enhance faecal excretion, reduced the half life of stored chlordane and enhanced the rate of recovery from toxic manifestations. The rationale for the use of cholestyramine lies on the biliary-enterohepatic circulation of chlordane, the anion-exchange resin binding the secreted insecticide and retaining the bound agent in the lumen of the intestinal for faecal excretion. The application of this finding to other organochlorine insecticides is dependent on the extent of biliary secretion of the agents and/or their metabolites. It is possible that cholestyramine might prove efficacious in treating organochlorine insecticide intoxications.
In eye exposure, the exposed eyes should be irrigated with copious amounts of water for at least 15 minutes. If irritation, pain, swelling, lacrimation or photophobia persist after 15 minutes of irrigation, an opthalmic examination should be performed.
Under dermal exposure to a highly concentrated organochlorine, the chemical is more effectively removed by soap and water compared to water alone. Again oil-based solvents should be avoided as they may enhance the dermal absorption of organochlorine insecticide.
Poisoning Emergency/ Information
-
Mon-Fri8am-10pm
-
Sat, Sun & Public Holiday8am - 5pm
-
Telephone04 6536 999
-
Telegram chat

