1234567890
prn8099 - Number 14, August 1997
Louis Lasagna, a medical doctor and a professor at Tuft University, has been quoted as saying: "The mind of man has removed the stopper of the bottle from the medicine jar. The chemical genie formerly imprisoned within now stands before us. He is a spirit known to work miracles, but also wreak havoc - to improve life or destroy it. It is not clear that we are yet sufficiently wise to control the genie adequately. It is quite clear that we can never wish him back into the jar." The analogy of medicine to a genie is indeed interesting if fairly accurate.
Paracetamol is one of those many, albeit not quite as vengeful a genie. Even then, the havoc it is known to cause cannot be taken lightly, otherwise as noted by Lasagna, we are bound to lose control, being the genie it is. Of late the Drug Control Authority (DCA) has been fit to exercise one such control though not amounting to putting the genie back into the proverbial jar.
In its 73rd meeting, the DCA has decided to cancel the registration of all paracetamol 500mg/5ml liquid preparations, normally meant for children. This decision was taken after receiving three reports of paracetamol toxicity in children - one fatal - associated with the use of paracetamol in such a strength. The 'unintentional' overdose occurred as a result of using paracetamol in four times the required dose, that is 500mg/5ml rather than the 120mg/5ml preparation. To prevent the recurrence of similar incidence, the DCA decided not to register any paracetamol liquid preparation with this strength. Six months period has been given for companies to remove the affected products already on the market. This grace period should have already expired.
Paracetamol is indeed a friendly chemical genie. It has been dubbed as one of the safest product on the market. This means that the therapeutic benefits that could be derived from it far outweigh the potential risk inherent in the product, provided it is used as recommended. It is so safe that its sales in Malaysia ranked among one of the top, at least for the one popular brand name associated with it. There is no wonder therefore that almost every manufacturer wanted to be on the bandwagon. As a testimony to this, today, all in all the number of products registered with the DCA known to contain this active ingredient is said to be about 250 types, each with a different 'pet genie' name and strength. It is also not suprising that most of these are not even known to many professionals and the public alike - begging the question as to the need to have such a long list of paracetamol. If combination products containing paracetamol are taken into consideration, the number will easily swell to about 100 more making it perhaps one of the largest product range in the Malaysian market.
Each of the genie can take various features ranging from tablets and capsules to injections (a form rarely seen in other developed countries like UK and US). It can also exist in different colours, shapes and sizes sometimes for seemingly different purposes - regular, children and menstrual. It is also noted by DCA to be a major component in many combination products, particularly cough and cold remedies. Such a variation in features make the genie paracetamol even more difficult to discern be it by the public or the professionals, true to the very nature of a genie. In a sense, it is an indication of what the pharmaceutical trade is all about, being omnipotent and omnipresent as well. A trade so lucrative that even in times of recession it seldom faces an economic downturn in the proportion encountered by their trading counterparts.
The reason for this is easy to understand. Sickness is not correlated directly to any form of recessions. if at all, more people will be 'sick' then! So the demand will still be there if not greater. Moreover, take paracetamol for example, it costs a fraction of the cost to make, yet they are sold on average at least ten times more to the consumer regardless of the brand names. Indeed, the best-seller in the class fetched a prize almost twice the average price-tag. Again this perhaps is a reflection of today's consumer preference, namely, "the more expensive is the product, the better it is". Such rule of thumbs applies to almost all medicines - a sad reality of modern day medicine! And this is bound to stay, especially under the so-called privatized health care.
It's magic
Called anything a medicine, and give it a strange sounding name; there will be a niche for it to be sold direct and indirectly. Medical products are known to create its own market needs - sometimes artificially induced. All the same, it would be sufficient to generate some income for the manufacturer, distributor and retailer alike. Thus, there are those who will slave for it, no matter at whose expense. The ultimate potential loser of course would be the consumer be it terms of health or money, or as quite often not realised - the emotional consequences. The worst-case scenario would of course be the fake and counterfeit medicines being dumped into the market. For example the settlers in the Felda and Felcra schemes, villages and estates were at the receiving end. Paracetamol is one of them. Such a marketing 'strategy' apparently is an attractive proposition to the unscrupulous. Today intermittent seizures of fake paracetamol tablets are still being reported in the local dailies. In a population where the level of awareness is consistently low, substandard products could easily make an in road thanks in parts to the aggressive direct-selling approaches practised in this country. Recently fake paracetamol were spotted again this time on 'wheels.'
Not withstanding this, by and large there will always be a captive audience for drugs like paracetamol. Once sold many would stay loyal with what seems to works, psychologically or otherwise. Moreover, like in all things it is better to deal with the genie we know (or at least we think we know) than the ones we don't. But then who really cares how a medicine actually works? For some, the more unexplained it is, the better it would be; pandering almost into the world of magic! This is perhaps why the need for information about medicine is often not given priority, so that the magical aura remains intact if not enhanced. As mentioned by Thomas Szasz in The Second Sin, (1973):
Moreover, a genie like paracetamol has never lost its magic. It seems to be good for all times. Like any magic, paracetamol is perceived to work wonders and it can never go wrong, least still create harmful effects. In fact, the brand name of at least one type of paracetamol is a household word in many Malaysian families, with most storing it casually at home without even realising that the medicine can kill. Few realise that it has actually killed since such information is usually not made public. The wisdom professed by the noted fifteenth century Swiss physician, Paracelsus, that differentiated medicines from poisons seems to have been altogether lost. For it was Paracelsus who wrote: "All things are poison and nothing is without poison. It is the dose only that makes a thing not a poison." But to the minds of many, paracetamol is excluded from this basic tenet of modern toxicology. There just isn't any possibility for any innocent genie like paracetamol turning itself into something so damning!
Self-poisoning
Consequently, the health impact in terms of poisoning is far and wide. So much so in 1995, the Committee on Safety of Medicines of United Kingdom issued a statement to emphasize that, although paracetamol is a safe and effective analgesic at recommended doses, it has become the most frequently used in 'self-poisoning'. According to the statement quoted in WHO Drug Information 10(1):44, 1996, unintentional overdosage has also occurred as a result of persons taking two or more preparations containing paracetamol at the same time. While the extent of polypharmacy of this nature has yet to be fully verified in the Malaysian context, the DCA already took the appropriate step in 1993 to minimize the problem. It requires all paracetamol-containing preparations to have on their packages the following warning label: "This preparation contains PARACETAMOL. Do not take any other paracetamol containing medicines at the same time."
Be that as it may, last August, the president of Malaysian Society of Gastroenterology and Hepatology Association (MSGHA) sounded a warning saying that cases referred to major hospitals like such as in Kuala Lumpur were showing trend of teenage girls using paracetamol "as a form of suicidal attempt." Indeed, last year saw a tragic death of a senior local university student arising from paracetamol overdose, most likely intentional. And according to the reports of the Chemistry department of Malaysia, paracetamol is among the top 5 substances found in the samples from poisoning cases analysed in 1994 and 1995. This may well be only the tip of the iceberg. One has not even begun to talk about parasuicidal cases such as the one that occurred in the UK, as late as December last year. A 14-year old schoolgirl, apparently took paracetamol just to be sick enough to skip classes for a few days after being tauted and labeled as a 'zombie' and 'Mortica' by her classmates; but accidentally being overdosed and died of liver failure. Again to quote the president of MSGHA while liver failure due to paracetamol is common in the West, "now it seems to be increasing in Malaysia."
| Poison | 1994 | 1995 |
| Paraquat | 294 | |
| Paracetamol | ||
| Methyl salicylate/salicylic acid | ||
| Benzodiazepines | ||
| Malathion |
There are other casual anecdotal reports on the non-medical use of paracetamol among some adolescent. How about paracetamol for 'breakfast' or just plain living on a 'paracetamol' diet. relevant to those would be a recent report that suggested 'fasting' could potentiate the hepatic toxicity of paracetamol even a generally non-toxic doses (4-10g daily for several days). Then again what about its use with alcohol or better still concocted with some carbonated drinks? The 'magical' thing about all these is that no one seems to notice the subtle sleight of hand.
More importantly it seems to underscore some unhealthy socio-medical norms that have been left unattended far too long. One outstanding problem is the tendency to ignore patients' right to information and consumer education as part of a larger context of drug-seeking behaviour. All over the country the inherent medical practice largely stops short at the prescribing and dispensing of medicines ignoring the need of patients to know anything substantial about their prized medications. Practitioners in many cases hurriedly send their patient away with a sachet of the drugs, quite accurately depicting the words of a nineteenth-century physician: "Make haste to use your remedies, before they lose the power of working miracles."
A genie for every ill
This tendency of widespread drug use goes on to create another adage: 'a pill for every ill', one which is also fast becoming a norm among the population at large. Whatever the situation, there is no doubt that the dangers in the misuse of medicines, in the Malaysian context, are lurking around waiting to strike at the first chance of negligence, ignorance, arrogance, and pure greed as the case may be. In a recent meeting on adverse drug reactions (ADR) held in Kuala Lumpur for example, cases of paracetamol-induced liver failure were again highlighted, bearing in mind that the level of reporting of ADR among practitioners are generally very much to be desired. To add to this, practitioners including doctors and pharmacists seldom warn patients, or counsel them about home medicines, with the view to inform and avoid potential risk in misusing them, namely, taking more than the required dose or more than one preparations containing the same drug.
Thus, very few people are given, or even bother to spend time getting the information that rightly should be explained to them. Apart from the 'how', the 'what', 'why' and even 'when' are usually glossed over if at all. Consequently, many are still in the dark when inquired about their medications, even for a chemical genie as pal-ly as paracetamol. In fact, it would not be at all suprising if the patient or consumer is even unaware of the maximum daily doses that must not be exceeded. What about the inherent dangers that exist in all medicines? How many then really knows what to do when encountered with a possible adverse effect especially on prolonged use of the drug. In 1994, a study published in The New England Journal of Medicine suggests that the user of paracetamol of more than 104 pills a year are up to twice as likely as those who take fewer than 104 to develop end-stage kidney failure. Those who take a cumulative lifetime dose of 5,000 or more pills are nearly 9 times more likely to develop kidney failure than those who take fewer than 1,000. So powerful was the effect of long-term paracetamol use that the drug appeared to cause up to 10 percent of all cases of kidney failure in the United States, the researchers reported. The prevailing myth however is still that drugs like paracetamol are entirely safety and good for all occasions. This is further reinforced by their widespread availability and accessibility throughout the country. According to a recent study conducted by researchers from Oxford, UK, the most common reason for patients deliberately choosing paracetamol is availability and being well aware of the dangers in the drug overdose. This was revealed when 80 patients with paracetamol self-poisoning were interviewed.
Locally, it is possible that the problem associated with drugs like paracetamol are much greater than what actually meets the eye, given the prevalent habits of doctor- and pharmacy-hopping by many patients, the generally poor and inadequate standard of labeling of dispensed medicines, the tendency to hoard 'old' drugs, the overall low level of awareness, and now the up trend in paracetamol (mis-)use. After all paracetamol could be sold to all and sundry by almost every vendor and outlet licensed or otherwise.
Thus looking at the potential problem ahead, every option must be seriously considered in our attempt to safeguard public interest, since paracetamol is no longer the gentle genie that we once knew. The genie named paracetamol is beginning to rear its ugly ahead and showing its true colour. While the previous decisions taken by DCA are steps in the right direction, there are other considerations that are worthwhile pondering upon. Foremost is to dismantle the prevailing myths and trends that surround the use of medicine like paracetamol.
In support of this, there is an urgent need to reconsider the sheer number of products currently available in the local market, apart from the question of 'unguarded' distribution - accessibility, availability and overusage of such a product. Locally, there are still packages of paracetamol containing more than 10 gram of total weight; thus increasing the real risk of fatal reactions. Such packaging should be prohibited so that the potential for abuse could be reduced. For persons who are prone to suicidal attempts, it is also worth considering making available a preparation containing a combination of paracetamol and methionine as suggested by the UK Committee on Safety of Medicines. This is because paracetamol overdose is said to be rapidly fatal unless promptly treated with methionine or N-acetylcysteine.
PRN CONSULT 
Review of Paracetamol Poisoning
Rahmat Awang, Pharm.D
Painkillers are generally available over-the-counter. The range include aspirin, paracetamol and non-steroidal anti-inflammatory drugs. In children, paracetamol is the drugs of choice as an analgesic/antipyretic because it is relatively safe and easily accessible. In many similar instances it is also the preferred drug for adults. Unless properly used and stored such drugs can result in pisoning especially involving children. PRN CONSULT reviews some of the salient points in paracetamol poisoning. Paracetamol (acetaminophen, N-acetyl-p-aminophenol), is a major metabolite of phenacetin and acetanilide.
In some countries like the US, paracetamol accounted for 70% of the annual reported poisoning incidences and while in England, it is the leading cause of death from overdose, accounting for about 150 150 cases annually. Over the past few years, paracetamol has also been reported in some poisoning exposure in the country.
Should we be alarned when somebody ingests an overdose of paracetamol?
Yes! Paracetamol is primarily hepatotoxic and may be fatal. however, if managed early, the likelihood of such consequences may be reduced.
An overdose of paracetamol can cause serious liver injury especially if the amount ingested is more than 140mg/kg in children or more than 6-7 gm in adults. Ingestion of more than 10mg (20 tablets of 500mcg each) in adult may in fact be fatal. The risk for hepatotoxicity may even be increased if the patient also drinks alcohol, and/or on drugs that interacts with paracetamol such as barbiturates and other enzyme inducers.
How does the poisoning manifest itself?
Hepatotoxicity may be evident as late as day 4 from the time of ingestion. The manifestations associated with paracetamol poisoning may develop in 4 phases. Phase 1 which is between 1/2 to 24 hours post-ingestion may be seen with patient complaining of anorexia, nausea, vomiting and diaphoresis. Children however may look pale, quite ill and drowsy. These symptoms subside in phase 2, between day 1 and 3. Instead, patient may complain of right upper quadrant pain if there is any hepatic injury. Clinical laboratory tests when carried out may show elevation of SGPT, SGOT, LDH, bilirubin and prolongation of PT. Renal function may decline but BUN remains within normal limits. Following this, the patient may develop jaundice, coagulation defects and renal failure in day 3-5 (phase 3). Myocardial damage though has been reported is rare. Hepatic encephalopathy has also been observed. Nausea and vomiting may reappear. Biopsy may reveal centrilobular necrosis. Hepatic failure may result in death. If damage is reversible, complete resolution may occur in day 4 to week 2 (phase 4).
How can one predict the likelihood of hepatoxicity from paracetamol poisoning?
One approach which is simple but crude is to determine how much and how long ago was the drug taken. If the amount ingested is as stated above, then the likelihood is great, especially when the presence of signs and symptoms are evident. Patients admitted into the hospital should have their CBC, platelets, PT, bilirubin, BUN, elctrolytes, glucose, SGOT, SGOT, alkaline phosphatase profiles checked.
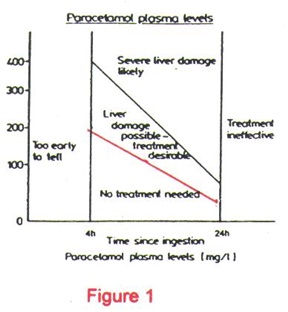
Another more reliable approach is to determine the paracetamol plasma level and then plotting this value onto the Rumack-Matthew Nomogram. The nomogram provides a good correlation between the paracetamol plasma level with the risk of hepatotoxicity. For example, a 4-hpur paracetamolplasma level at various concentrations have been correlated with the following risk:
| >300mcg/ml | liver damage* and fatalities very likely
25% chance of developing acute renal failure |
| 250-300mcg/ml | 40% chance of developing liver damage* |
| 150-250mcg/ml | 25% chance of developing liver damage* |
| 120-150mcg/ml | 5% chance of developing liver damage* |
| <120mcg/ml | relatively non-toxic |
* Liver damage is indicated by plasma SGOT or SGPT level of greater than 40 IU/L, a PT of 1.3 times normal and plasma bilirubin > 1mg/dl
It is therefore highly desirable to draw the paracetamol plasma level when the amount ingested is close to or more than the amount needed to cause hepatic injury. this holds true if the timing for plasma level determination is appropriate i.e. between 4 and 16 hours post-ingestion.
Another approach is to determine the half-life of paracetamol. Plasma half-life for paracetamol in normals is about 1-2 hours. If half-life is more than 4 hours, it may be suggestive of hepatotoxicity.
How does one uses the Rumack-Matthew Nomogram? What precautions does one have to take in interpreting the information?
The Rumack-Matthew Nomogram estimates the potential for hepatotoxicity from paracetamol poisoning. In addition, it is also used to indicate the need for N-acetylcysteine (NAC) therapy. It is based on a semi-logarithmic plot of plasma paracetamol levels vs time. A plasma level that falls above the red line indicates a pitential for toxicity and requires NAC treatment. Anyone who uses this nomogram however, has to understand that the nomogram is applicable only when the poisoning involves a single acute ingestion and that the blood level is drawn between 4 and 16 hours. Blood levels drawn before 4 hours may not represent peak levels since absorption is not complete and those dwarn after 16 hours may not be predictive of potential hepatotoxicity or the need for NAC therapy.
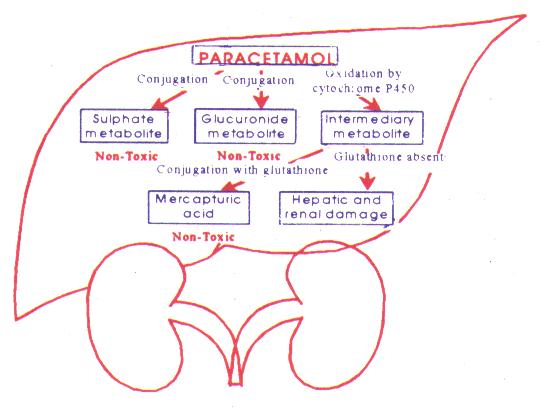
How does paracetamol result in hepatotoxicity?
Paracetamol is rapidly absorbed and metabolised by the liver primarily to sulfate and a glucuronide metabolites. Depletion of hepatic glutathione leads to the formation of toxic metabolites (? N-acetyl-benzoquinoneimine) which bind to hepatic macromolecules resulting in hepatic necrosis.
How does one manage paracetamol poisoning case?
In cases involving recent substantial ingestion, emesis is indicated unless the patient could rapidly become obtunded, comatose, convulsing. Emesis is most effective if initiated within 30 minutes. If available, syrup of ipecac at a dose of 30 ml in an adult or 15ml in a child of 1-12 years old is recommended. Charcoal administered with or without gastric lavage is also a preferred method of decontamination. However, its use may delay initiation of oral NAC since the antidote may be adsorbed by the charcoal rendering NAC ineffective.
NAC is an effective antidote for paracetamol poisoning when indicated. Dosing regimen for oral NAC is in the form of a 5% solution in asoft drink or juice starting with a loading dose of 140mg/kg followed by a maintenance dose of 70mg/kg every 4 hours for a total of 17 doses. IV administration of NAC can also be used.
The following situations warrant the use of NAC:
- if initial plasma paracetamol level is toxic on the nomogram. The therapy should be continued until the entire course is completed even if subsequent levels falls below the treatment line.
- if a toxic dose (7.5gms) is suspected to have been ingested within 16 hours of ingestion. Some Poison Centre recommend NAC therapy be given even up to 24 hours post-ingestion. Administration of NAC should never be delayed for lack of a paracetamol level. Loading dose should be administered but should be discontinued if level is below the nomogram treatment line.
- if paracetamol is below half-life is more than 4 hours.
Side-effects associated with the use of NAC include bronchospasm and anaphylaxis. Anaphylactic reactions may be life-threatening and thus treatment should be made readily available.
Poisoning Emergency/ Information
-
Mon-Fri8am-10pm
-
Sat, Sun & Public Holiday8am - 5pm
-
Telephone04 6536 999
-
Telegram chat

